The ills of pills
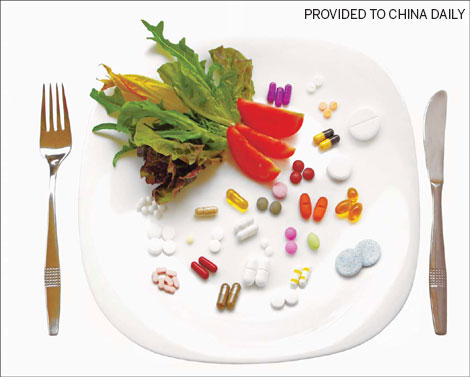
Taking multivitamins could actually increase the likelihood of dying prematurely, new findings appear to suggest.
Women taking multivitamins don't live longer than those who get their nutrients from food alone, a new US study shows.
In fact, they appear to have slightly higher death rates, researchers have found.
"There is very little evidence showing that common dietary supplements would be beneficial in preventing major chronic diseases," says Dr Jaakko Mursu of the University of Minnesota in Minneapolis, who worked on the new study.
"Unless you are deficient, there is hardly any reason to take them," he says.
About half of adult Americans take dietary supplements, and the industry now boasts of annual sales as high as $20 billion.
Yet research suggests that some of the largely unregulated substances - such as vitamins A and E - could be harmful in high doses, according to an editorial published along with the new findings in the Archives of Internal Medicine.
"The belief that antioxidant supplements are beneficial seems likely to have resulted from a collective error," Dr Goran Bjelakovic of the University of Nis in Serbia and Dr Christian Gluud of Rigshospitalet in Copenhagen write. "Perhaps oxidative stress is one of the keys to extension of our life span."
Mursu and his colleagues used data from nearly 39,000 older women who participated in the Iowa Women's Health Study and filled out questionnaires starting in 1986.
The survey asked about use of multivitamins, vitamins A, C, D and E as well as beta-carotene, B vitamins and minerals such as calcium, copper, magnesium, selenium and zinc.
During the study, supplements became increasingly popular: Between 1986 and 2004, the proportion of women who said they took one or more jumped from 63 percent to 85 percent.
Only calcium supplements were linked to a lower risk of death over 19 years of follow-up, with 37 percent of users dying compared to 43 percent of non-users. That link held up even after considering that women taking supplements had a healthier lifestyle than the rest.
By contrast, women taking other supplements did not live longer. For instance, 41 percent of multivitamin users died versus 40 percent of nonusers - and the gap became even wider when adjusting the numbers based on health problems like diabetes, high blood pressure and overweight in the two groups.
Mursu says he expects his findings will be true for men as well, adding that they jibe with earlier research hinting that dietary supplements do little good in Western countries where vitamin deficiency is not common.
One possible exception is vitamin D, which one recent study suggests may help women live a little longer.
Mursu also cautions that his study doesn't prove supplements cause harm.
"I would rather conclude that there is no evidence for benefits," he says.
The 2010 US dietary guidelines recommend getting nutrients from foods, not supplements.
However, women of reproductive age group are advised to get extra folic acid and those who are pregnant may want to take iron supplements if their doctor suggests it. The guidelines also urge people 50 and older to get extra vitamin B12 from fortified foods or supplements.
Duffy MacKay of the Council for Responsible Nutrition, a trade association representing manufacturers and ingredient suppliers of dietary supplements, disagrees with the researchers' conclusion that doctors should only recommend supplements to people with deficiencies.
He adds that in the case of iron, women on high doses may have underlying conditions that could explain their higher death rates.
While Mursu acknowledges that shortcoming, he says it is unlikely to be relevant for multivitamins, which usually aren't prescribed by a doctor.
Short of getting sick, he says it's hard to know if you are getting enough vitamins and minerals - and screening everybody would be prohibitively expensive.
His advice?
"Include as many vegetables and as much fruit as you can. There is hardly any reason to limit those, and they contain a whole lot of vitamins and minerals."
Reuters