DNA test for rare disorders on rise
|
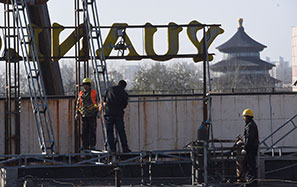
Inexpensive gene sequencing is attracting parents seeking answers about rare disorders like those of Lillian Bosley, above with her father, Sam; and Jacob, far left, and Eli Sukin. Michael Stravato for The New York Times Matt Roth for The New York Times |
Debra Sukin and her husband were determined to take no chances with her second pregnancy. Their first child, Jacob, who had a serious genetic disorder, did not babble when he was a year old and had severe developmental delays. So the second time around, Ms. Sukin had what was then the most advanced prenatal testing.
The test found no sign of Angelman syndrome, the rare genetic disorder that had struck Jacob. But as months passed, Eli was not crawling or walking or babbling at ages when other babies were.
"Whatever the milestones were, my son was not meeting them," Ms. Sukin said.
Desperate to find out what is wrong with Eli, now 8, the Sukins, of The Woodlands, Texas, have become pioneers in a new kind of testing that is proving helpful in diagnosing neurological illnesses in children. Scientists sequence all of a patient's genes, systematically searching for disease-causing mutations.
A few years ago, this sort of test was so difficult and expensive that it was generally only available to participants in research projects. But the price has plunged from tens of thousands of dollars to $7,000 to $9,000 for a family, and American health insurance companies will usually pay for the testing.
Demand has soared - at Baylor College of Medicine in Waco, Texas, for example, scientists analyzed 5 to 10 DNA sequences a month when the program started in November 2011. Now they are doing more than 130 analyses a month.
Even if there is no treatment, there is almost always some benefit to diagnosis, geneticists say. It can give patients a prognosis. It can also ease the processing of medical claims, qualifying for special education services and learning whether subsequent children might be at risk.
Experts caution that sequencing finds a genetic aberration in only about 25 to 30 percent of cases. About 3 percent of patients end up with better management of their disorder. About 1 percent get a treatment and a major benefit.
"People come to us with huge expectations," said Dr. William A. Gahl, who directs the National Institutes of Health program. "They think, 'You will take my DNA and find the causes and give me a treatment.' "
"We give the impression that we can do these things because we only publish our successes," Dr. Gahl said, adding that when patients come to him, "we try to make expectations realistic."
DNA sequencing was not available when Debra and Steven Sukin began trying to find out what was wrong with Eli. When he was 3, they tried microarray analysis, a genetic test that is nowhere near as sensitive as sequencing. It detected no problems.
But in November 2011, when Eli was 6, Ms. Sukin consulted Dr. Arthur L. Beaudet, a medical geneticist at Baylor. "Is there a protein missing?" she recalled asking him. "Is there something biochemical we could be missing?"
By then, DNA sequencing had come of age. Dr. Beaudet said that Eli was a great candidate, and it turned out that the new procedure held an answer.
A single DNA base was altered in a gene called CASK, resulting in a disorder so rare that there are fewer than 10 cases in the world's medical literature.
"It really became definitive for my husband and me," Ms. Sukin said. "We would need to do lifelong planning for dependent care for the rest of his life."
The typical patient with a mystery disease has neurological problems, and is often a baby or a child. Cures are rare, even if the gene defect is known.
Many patients are like 13-year-old Lillian Bosley, who has never learned to speak. Her hands and feet are turned inward. Her brain is malformed. She has severe developmental delays, seizures and vision problems.
Lillian's parents, Sam and Michelle Bosley of Frederick, Maryland, stumbled onto gene sequencing. It did not give them a diagnosis.
Mr. Bosley, meanwhile, is hopeful but resigned.
"In the end, I don't know that it would change anything," he said. "Maybe it is one of life's mysteries."
But the experience of the Beerys of San Diego raises the hopes of other families.
Retta and Joe Beery's twins, born in 1996, were not meeting developmental milestones.
At 1 year, Alexis and Noah could not crawl. Their muscle tone was so poor that anyone who held them had to support their backs. They vomited profusely every day.
A diagnosis of cerebral palsy turned out to be wrong.
The answer came in August 2010, when doctors at Baylor agreed to sequence the twins' entire genome as part of a research program. They discovered that Alexis and Noah had an extremely rare mutation in a gene, SPR, that knocked out synthesis of both dopamine and another neurotransmitter, serotonin.
The twins started taking 5-hydroxytryptophan, which the body converts to serotonin, along with L-dopa, a drug used to treat Parkinson's disease. Alexis, who had been unable to participate in any sport because of her difficulty breathing, was running track three weeks later. Noah's tremors went away. His handwriting and his eye-hand coordination improved.
Ms. Beery has made it her mission to tell her children's story and to encourage families to seek testing. But Dr. Beaudet, the Baylor geneticist, cautions that very few families get such a happy ending.
"Theirs," he said of the Beerys, "is the world's poster story for this kind of activity."
The New York Times